Information for Injured Adults
Information for Injured Adults
If you are an adult coping with a recent injury, you may have a lot of questions about what to be thinking about as you recover. Apart from the physical side of the injury, there are often accompanying emotional challenges. It is important to remember that recovery from an injury involves not only physical recovery, but also emotional and mental recovery. Our goal is to provide you with information, tips, and resources to help you as you adapt to this recent challenge.
Stress and Injury:

What aspects of an injury and hospital visit might be stressful?
Multiple aspects of an injury and/or the hospital experience can impact your reactions to the event. These can include:
- The type of injury you experienced
- How you got injured
- The types of treatments you received in the hospital
- Shock or feelings of loss of control associated with the injury
- Life-altering medical complications or lifestyle changes related to your injury
- Interactions with emergency responders or law enforcement
- Receiving medical interventions that you did not expect or understand
- Conditions of the hospital environment
- Pain associated with the injury
What types of changes and challenges might I experience?

It is natural for people to have some difficult reactions after a medical trauma. These reactions will naturally decrease over time for most people. Here are some common reactions:
- Difficulty sleeping, working or socializing like you used to
- Blaming yourself for what happened, even when others tell you that you are not to blame
- New and uncomfortable sensations in your body
- Difficulties with attention, memory, or concentration
- Pain
- Emotional changes (anger, sadness, fear)
- Thinking a lot about the injury event itself, and trying to make sense of what happened or why it happened
Changes in Thoughts, Beliefs, and Attitudes
Following a physical injury, we focus on cognitions about ourselves, the world, and the injury itself. Cognitions sometimes change after a traumatic event like a physical injury. These cognitions might include:
- Thoughts about the world being less safe
- New beliefs about people being more or less trustworthy
- Changes in views of your own self-worth and future prospects
- Guilt related to the injury event (for example, believing that the event was your fault, or ‘survivor guilt’ if you lived through the accident and someone else was killed)
- Thoughts that your life will never be the same
- Identifying with others who have experienced something similar
- Decreased self-confidence
These cognitions can sometimes be very persistent and difficult to get rid of, and sometimes come in the form of racing thoughts or thinking about the event over and over again.
How do I manage these changes in my thoughts and beliefs?
There are many ways to increase awareness of your thinking patterns and develop more helpful and flexible thinking.
Changes in Feelings and Emotions
The emotional reactions you experience after a stressful event can sometimes be difficult to manage. These feelings can include:
- Anxiety or fear (including fear of getting injured again)
- Guilt
- Feeling joyful or grateful that you survived
- Anger
- Sadness
- Helplessness
- Feeling unreal or detached
- Numbness
- Disorientation
- Feeling out of control
- Denial
- Feeling constricted
- Feeling overwhelmed
- Loneliness or isolation
- Disappointment
- Frustration
- Gratitude that nothing worse happened
When you are experiencing difficult emotions, there are things you can do to make the emotions more manageable:
- Talk with a trusted friend or family member about how you are feeling. Let them know how you are feeling and how they can help.
- Do things that help you to feel better when you are having a hard time- time outside, exercise, listening to music, prayer, playing a board game, watching a movie, reading a good book, and spending casual time with friends and family are just some of the options to consider.
- Remember that these emotions may feel overwhelming now, but they are likely to improve and become more manageable, especially if you seek support, learn tools for managing stress, and focus on basic needs such as sleep.
Behavior Changes
Behavioral reactions are important to be aware of because they can affect our relationships or slow down our recovery process. Behavioral changes may include:
- Restlessness
- Changes in sleep and appetite
- Difficulty expressing oneself
- Being argumentative or aggressive
- Increased use of alcohol, drugs, and tobacco
- Withdrawing from loved ones
- Avoiding people, places, thoughts, or memories that remind you of the event
- Changes in performance and behavior at work. Click here to read our tips for communicating with your employer.
- Having nightmares
- Increased engagement with religious or spiritual activities
It is important to remember that some behavior changes are normal after an injury. After all, you have just been through a very stressful experience. It is important to be aware of any changes in how you are acting and how those changes may be impacting your relationships, work abilities, and other life activities. Work on using the skills and techniques you are developing, and seek help from a provider if you need professional support.
Physical and Body Reactions
The physical reactions you experience after an injury can be confusing, because it can be difficult to tell if they relate to your recent injuries and related medical symptoms or to the emotional and social impacts of the stressful event. Often, our emotions are connected to physical symptoms. For example, if you feel anxious you may also feel an elevated heartbeat. Physical reactions may include:
- Nausea or upset stomach
- Sweating or shivering
- Feeling faint
- Muscle tremors or uncontrollable shaking
- Changes in appetite
- Elevated heartbeat, respiration, and blood pressure
- Extreme fatigue or exhaustion
- Feeling ‘jumpy’
- Experiencing pain
Exercise, diet, proper sleep, talking with your medical provider, and seeking support from family and friends can all make these symptoms more manageable.
Memory and Concentration Changes
After an injury or other stressful event you may notice changes in things like memory, attention, concentration or ability to make decisions. Often, experiencing pain or struggling with emotional challenges affects our cognitive functioning as well. These difficulties could include:
- Difficulty concentrating
- Memory problems
- Feeling like time is moving in “slow motion”
- Confusion
There are many ways to manage these changes, and it is important to know that for most people these problems get better within a few weeks to a few months. We put together some tips for managing these types of problems.
As you can see from this list, not all reactions are negative! Sometimes after a stressful event people feel more clear about what is important to them and feel a renewed connection with their loved ones. While this is not true for everyone, it can be helpful to notice any positive changes that may be happening in the midst of the challenges you are experiencing.
How long will these new emotional challenges last?

Life can feel overwhelming in the weeks following an injury, and setting realistic expectations of recovery may help you cope and adjust to challenges. While there is no clear answer to how long recovery will take, in most cases, it will take a few weeks to a few months to feel like you have adjusted to the injury. If you use helpful coping techniques, your recovery can happen more quickly and effectively.
Differences in Recovery after Medical Trauma
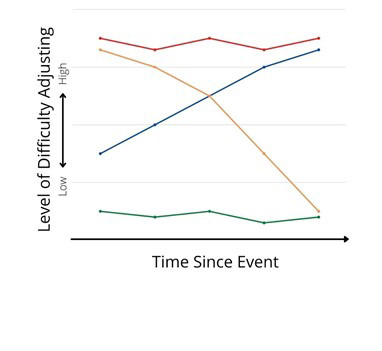
The figure below shows different trajectories of recovery after an injury or stressful event.
The red line shows that 10-30% of people continue to experience chronic distress for a long time after an injury.
The blue line shows that a very small number of people (5-10%) experienced delayed onset of symptoms.
Notice that the majority are resilient or recover quickly. In other words, most people’s recovery process after an injury looks like either the green line or the yellow line on this graph.
The green line shows a recovery that involves low levels of emotional distress immediately after the event, and also into the future.
The yellow line shows a high level of symptoms immediately after the injury, but a clear return to low levels of symptoms as time goes on. In other words, 50-90% of people have a low level of distress within a few weeks to a few months after an injury.
It is important to note that emotional and behavioral recovery after an injury is not always predictable! There will likely be a mix of good days and hard days. Every person recovers differently, both physically and emotionally.
FAQs
- Talk about what happened when and if you feel comfortable. One of the best ways to relieve difficult feelings and worries is to share them with someone you trust and feel supported by. Tips for talking to your Loved Ones about your Injury
- Use deep breathing. Deep breathing can help you manage your feelings, reduce pain, slow your heart rate, and lower blood pressure. Pain Management Techniques
- Take time to adjust. It can take time to get back into a regular routine. Make time to do things you enjoy, take things one day at a time and return to your normal schedule as much as possible as you are able
- Communicate with your employer when you are ready. Consider when and how you will return to work, and come up with a plan for communicating with your employer. Communicating with your Employer
- Try out some mental health apps. Apps like Virtual Hope Box, PTSD Coach, Family Coach, Move Forward, CBT-I Coach, Headspace and Woebot can also help you learn new coping skills but should not replace a mental health professional. Resources
- Remember that adapting to an injury involves medical/physical healing as well as emotional/mental recovery. It is a good idea to be aware of all of the ways the injury has impacted your life. It is important to note that for some people, the emotional and mental healing can take longer than the physical healing.
- Keep a positive but realistic outlook. Take good care of yourself (get sleep, seek support) and remember that for most people, things start to get better with time, medical treatment, focusing on caring for oneself, and accepting help from others.
- Talk with your medical providers about what to expect. Ask your medical providers about what the recovery process is likely to be like, what challenges are likely to come up, and when you can start resuming normal activities. Click here for information about communicating with medical providers
- Focus on daily progress - don’t go too fast or too slow in your recovery process. You don’t want to rush into activities before you are ready- this can lead to frustration, sadness, and a slower recovery process! On the other hand, if you get out of the habit for too long, it can be more difficult to get back into your daily routines and can slow down your recovery. Talk to your providers about when you can start getting back to daily tasks, and work with them to keep on the path of healing.
- Expect to experience a variety of emotions, with gradual improvement over time. It is likely that you will have both good days and bad days, both frustrating moments and positive experiences as you recover from injury. Sadness, hope, stress, humor, and frustration can all be a part of the injury recovery process
Changes after an injury are common. Most people recover after a few weeks or months. If these changes last more than a few weeks and interfere with everyday life, support may be needed. Feel free to email us at bright@uccs.edu if you have questions and we will provide information about additional electronic resources available to you, such as our text messaging support program and others, and we will also provide mental health treatment referrals if we can.
Here are some examples of situations in which seeking extra support, such as psychotherapy, may be a good idea:
- Intense memories: You find yourself repeatedly going over the details of the trauma in your head. Something you see, hear, smell, touch, or taste may cause you to feel the same feelings you did when the event happened.
- Avoidance: You avoid things, places, and people that remind you of the event. You may not want to go back to the hospital, see your doctor again, or take medications.
- Persistent symptoms: You experience ongoing and lasting changes in the way you think and feel.
- Nervousness: You feel very nervous. You may feel “on edge,” have a hard time falling asleep, or have trouble controlling pain. You may suddenly become angry or irritable with yourself or others.
If you continue to experience any number of these reactions after a few weeks, it is a good idea to talk to a medical or mental health professional.
Charlie, age 34, was assaulted and robbed while walking home from work and was injured, including multiple fractures in his legs and several broken ribs.
Charlie initially experienced both medical symptoms and emotional/social challenges after this event. The medical symptoms included pain, difficulty breathing, and trouble sleeping. Charlie also experienced emotional challenges like anger/frustration, sadness, fear walking home from work, troubling memories and dreams, and feeling panicky in situations that remind him of the assault.
In the days following the event Charlie worried that these symptoms might be permanent and that they would never return to normal. This is an understandable feeling because Charlie’s symptoms were difficult to manage. But Charlie’s medical symptoms were significantly better within a few weeks, and Charlie was almost symptom-free within a few months.
The emotional and social challenges that Charlie experienced also resolved within a few months. This timeline is true for most people, though emotional recovery from a traumatic, life-threatening, and violent event like an assault can be more complex than recovery from an accidental injury.
Throughout the recovery period, Charlie focused on what could be done to recover healthfully. As Charlie explained…
"At first it was really hard. I thought about it all the time. One thing that really helped is I had a friend who had also been a victim of a mugging several years ago. But apart from talking about it with him, I didn't want to do anything. I was afraid to go out at night, and even afraid to walk home from work in the daylight, which was embarrassing. My friends wanted to go out and do things, but I just didn't feel like it. My friends and family kept saying it would make me feel better to get out, so finally I forced myself to do it. And sure enough, eventually it did help. The first time I went out I was nervous and sweaty, and honestly I didn’t have a good time. But my doctors warned me that if I kept avoiding things, it would get harder and harder to stop. It eventually got better from there. The more I went out with my friends, even at night, the less anxious I felt.
And the pain - it was bad at the beginning. The surgeries and rehab went fine, but the pain took a while to go away completely. At first, I would feel some pain in my leg, and then it would remind me of that night. Then I would feel scared and the pain would get worse - a vicious cycle. I tried some pain management techniques my doctors recommended. I have to admit, at first I thought they were kind of simple, even stupid, but I did them anyway. Simple things like deep breathing or visualization. At first I did notice that it helped a little bit. Probably the best part is it would distract me from actually thinking about the assault and I would notice the pain wasn’t as bad either. As the pain got better over time, the thoughts and feelings did too. And, the more I tried these things my doctors and therapist recommended, the more I noticed I had more control over my pain and my thoughts and feelings than I thought I had. It was pretty wild to realize I could even control my pain and control my anxiety. It wasn’t easy, and I imagine there are a lot of other people that have had it worse than I had it, but now I am back to doing what I used to do. I want to let other people know they also have the ability to get through something like this."